Alleviation of Acute Poisoning of Organophosphates in Humans-Juniper Publishers
JUNIPER PUBLISHERS-OPEN ACCESS ANATOMY PHYSIOLOGY & BIOCHEMISTRY INTERNATIONAL JOURNAL
Organophosphates (OPs) are used as pesticides and
developed as warfare nerve agents. Exposure to an organophosphate could
be lethal resulting in death due to respiratory failure. The mechanism
of organophosphate poisoning includes inhibition of the acetyl
cholinesterase (AChE) via phosphorylation of the hydroxyl group of
serine present at the active site of the enzyme. The inhibition of
acetyl cholinesterase (AChE) results in the accumulation of
acetylcholine (ACh) at cholinergic receptor sites, producing continuous
stimulation throughout the nervous systems. Several therapeutic agents
have been developed and used in the treatment of poisoning with OPs. For
example, pyridiniumoximes have been developed as therapeutic agents for
the treatment of poisoning by OPs. The mode of action of
pyridiniumoximes is by the reactivation of inhibited acetyl
cholinesterase. However, the universal broad spectrum oximes capable of
protecting against all known OPs, is still have to be investigated.
Presently, a combination of an antimuscarinic agent, e.g. atropine, an
AChE reactivators i.e. oximes and diazepam are used for the treatment of
organophosphate poisoning in humans. In spite of enormous efforts
devoted to the development of new AChEreactivators as antidotes against
poisoning with organophosphates, only four compounds so far have been
found their applications in human medicine. This article presents an
updated account of the available reports concerning the treatment of OP
poisoning and its alleviation.
Keywords: Pesticides; Organophosphate Poisoning; Antidote; Acetyl cholinesterase; Cholinergic; AlleviationAbbreviations: OP: Organophosphate; AChE: Acetylcholinesterase; ChE: Cholinesterases; Ach: acetylcholin
Introduction
Acetylcholinesterase (AChE) (EC 3.1.1.7) is the
primary cholinesterase belongs to carboxylesterase family . It is an
acetylhydrolase, found in many types of conducting tissues. AChE is also
found on the red blood cell membranes and blood plasma (EC 3.1.1.8,
ChE) [1]. The function of AChE is the termination of ACh at the
junctions of the various cholinergic nerve endings with their
post-synaptic sites which catalyzes the breakdown of acetylcholine that
function as neurotransmitters with very high catalytic activity. The
turn over number for AChE has been found to be about 25000 molecules of
acetylcholine (ACh) hydrolysed per second [2]. The AChE activity is
higher in motor neurons than in sensory neurons [3,4]. AChE exists in
multiple molecular forms with different oligomeric assembly but having
the same catalytic activities. The enzyme has been reported to be
membrane bound [5-7]. The active site of AChE has two sub sites -
anionic site and esteraticsubsite.
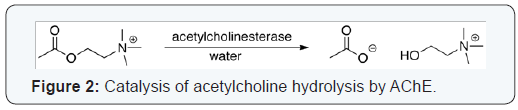
The esteraticsubsite contains the catalytic triad of
three amino acids: serine 200, histidine 440 and glutamate 327 similar
to the triad in other serine proteases except that the glutamate is the
third member rather than aspartate, where acetylcholine is hydrolyzed to
acetate and choline [8]. The hydrolysis reaction of the carboxyl ester
forms an acyl-enzyme and free choline. Then, the acyl-enzyme undergoes
nucleophilic attack by a water molecule, assisted by the histidine 440
group, liberating acetic acid and regenerating the free enzyme [9,10].
The mechanism of action of AChE has been elucidated in (Figure 1). The
anionic sub site accommodates the positive quaternary amine of
acetylcholine and other cationic substrates and inhibitors. The cationic
substrates are not bound by interaction of 14 aromatic amino residues
[11], which are highly conserved across different species [12]. Among
these aromatic amino acids the substitution of tryptophan 84 with
alanineresults in a 3000-fold decreased reactivity [13]. During
neurotransmission, ACh is released from presynaptic neuron into synaptic
cleft and binds to ACh
receptors on the post-synaptic membrane, relaying the signal.
AChE, also located on the post-synaptic membrane, terminates
the signal transmission by hydrolyzingACh. The liberated
choline is taken up again by the pre-synaptic neuron and ACh is
synthesized by combining with acetyl-CoA through the action of
choline acetyltransferase [14] (Figure 2).


Organophosphates (OPs), the esters of phosphoric acid, are a
class of irreversible AChE inhibitors. The cleavage of OP by AChE
leaves a phosphoryl group in the esteratic site, which is slow
to be hydrolyzed and can bound covalently. Carbamates, esters
of N-methyl carbamic acid, are reversible inhibitors of AChE
that hydrolyze in hours and occupy the esteratic site for short
periods of time (Figure 3). Presently, a combination of AChE
reactivators such as atropine and diazepam are used for the
treatment of OP poisoning. The drugs donepezil, galantamine,
and rivastigmine used in alzheimer disease are inhibitors of
AChE [9,15]. It has also been reported that some phytochemicals
such as tetrahydrocannabinol, the active ingredient of cannabis,
is a competitive inhibitor of AChE [16]. This article presents
an updated account of the reports available concerning the
alleviation of OP poisoning by some antidotes including atropine
and oximes.
Interaction of cholinesterases with organophosphates
The physiological role of AChE in blood is not understood, but
it was proposed that ChE may have roles in neurotransmission
and involved in other nervous system functions and in
neurodegenerative disorders [17]. In the presence of OPs, AChE
becomes progressively inhibited and is not further capable
of hydrolyzing ACh [18]. Consequently, ACh accumulates at
cholinergic receptor sites and produces excessive stimulation
of cholinergic receptors throughout the nervous systems. Both
substrate and inhibitors react covalently with the esterase in
essentially the same manner, because acetylation of the serine
residue at AChE catalytic site is analogous to phosphorylation.
Inhibited enzyme can be spontaneously reactivated at different
rates depending on the inhibitor. The variations in the acute
toxicity of OP are the result of their different chemical structures
and rates of spontaneous reactivation and aging. The aging
has the major clinical importance and an imperative problem
in the treatment of pesticide poisoning because aged form of
phosphorylated AChE is resistant to both spontaneous and
oxime-induced reactivation. Hence, recovery of inactivated AChE
function depends on relatively slow resynthesis of AChE during
aging thereby exerting higher level of toxicity as compared to
those at younger age.
Clinical presentation of OP poisoning
According to World Health Organization (WHO), in cases
of intoxication the signs and symptoms of acute poisoning with
OPs are predictable from their levels of AChE activity [19]. These
clinical features include sweating, lacrimation, rhinorrhea,
and abdominal cramps, salivation, respiratory difficulties,
dyspnea, cough, wheezing, fasciculations, bradycardia,
change in ECG, cyanosis, anorexia, nausea, vomiting, diarrhea,
involuntary urination and defecation, accompanied by
dizziness, tremulousness, confusion, ataxia, headache, tremors,
constriction sensation in the chest, twitching of facial muscles
and tongue, and fatigability finally into death. It has been reported
that even after survival of the patient with OP poisoning, there
would be mood swings, personality changes, aggressive events
and psychotic episodes [20,21]. Diagnosis is relatively based on
medical history, exposure circumstances, clinical presentation,
and laboratory tests. Erythrocyte AChE is identical to the enzyme
present in the target synapses and its levels are assumed to
reflect the effects of OPs in target organs. Thus, erythrocyte
AChE may be considered as a biomarker of neurotoxicity. Due
to pharmacokinetic reasons, it is difficult to know exactly, how
closely the AChE inhibition in erythrocytes reflects to that in
the nervous system since access to blood is always easier than brain. Thus, erythrocytes AChE inhibition may reflect altogether
a different message from that in brain [18].
Treatment of acute poisoning with Organophosphorus pesticides
Treatment of OP pesticide poisoning should begin with
decontamination and care must be taken not to contaminate
others.
Atropine
Atropine acts through blocking the effects of excess
concentrations of acetylcholine at cholinergic synapses following
OP inhibition of AChE. It has been reported that atropine may
prevent development of convulsions and brain damage induced
by certain OP [22]. The trial dose of atropine is 0.05 mg/kg
intravenously, should be given slowly over 3 min, and then
repeated every 5–10 min. In symptomatic children, intravenous
dose of 0.015–0.05 mg/kg atropine should be administered at
interval of every 15 min. Atropine may then be repeated at 15–
30 min intervals until the patient is atropinized (dilated pupils,
dry skin, and skin flushing) which should be maintained during
further treatment.
Diazepam
Benzodiazepines are central nervous system (CNS)
depressants, anxiolytics (antipanic or antianxiety agent)
and muscle relaxants. Marrs [23] in has reported that
benzodiazepines, including diazepam, alter GABA binding in
an allosteric fashion. The recommended dose of diazepam in
cases of OP poisoning is 5–10mg intravenously in the absence
of convulsions and 10–20mg intravenously in cases with
convulsions [22].
Oximes
The antidotal potency of pyridiniumoximes is primarily
attributed to their ability to reactivate phosphorylated
cholinesterases. Reactivation proceeds through the formation of
intermediate Michaelis-Menten complex leading to the formation
of stable phosphoryl residue bound to the hydroxyl group of
serine present at active site of AChE. The rate of reactivation
depends on structure of phosphoryl moiety bound to the enzyme,
source of the enzyme, rate of post inhibitory dealkylation and
concentration of oxime [24,25]. Pyridiniumoximes are effective
in the peripheral nervous system, but also have a penetration
across the blood–brain barrier [26] and therefore enable passage
of higher oxime concentrations into brain [27]. Pralidoxime
is not sufficiently effective in the treatment of OP pesticide
poisoning [28]. The inadequate initial treatment with oximes
may not be sufficiently effective in OP poisoning because oximes
are rapidly cleared from the body. Among the many classes of
oximes investigated with clinical application can be divided
in following groups: monopyridinium (PAM-2, pralidoxime),
bispyridiniumoximes (TMB-4, trimedoxime), obidoxime (LuH-6,
Toxogonin) and asoxime (HI-6).
Pralidoxime (PAM-2)
Sidell and Groff (1971) have shown that the pralidoxime
administered to human at a dose of 10 mg/kg by intramuscular
route, produced a plasma concentration of >4 mg/L within 5–10
min and maintained levels above this threshold for an hour
[29]. The PAM-2 iodide was given in combination with atropine
and diazepam, in the treatment of the victims of Tokyo sarin attack victims in 1995 [30]. However, PAM-2 should not be
recommended against poisoning with warfare nerve agents due
to its lack of efficacy [31].
Obidoxime
Obidoxime when administered to humans by intramuscular
route, it produced a plasma concentration >4 mg/L, from 5 min
after injection to 3 h [32]. Following high doses of obidoxime in
severely OP poisoned patients; occasional hepatotoxic effects
have been observed including increased serum transaminases
and jaundice [33].
Asoxime (HI-6)
Asoxime is considered to be a very promising
bispyridiniumoxime in treatment following exposure to
most nerve agents. Studies showed that Asoxime dosed by
intramuscular route reached plasma concentrations >4 mg/L
in 4–6 min [34]. According to Jovanovi´c et al. [35] asoxime did
not show any adverse effect on humans. The only disadvantage
of asoxime compared to other available oximes is its lack of
stability in aqueous solutions. Asoxime was considered to be
an effective antidote in treatment of patients poisoned with OP
insecticides [34].
Conclusion
The management of acute Organophosphate pesticide
poisoning in humans includes general (decontamination and
supportive measures) and specific treatment with atropine,
oximes (pralidoxime, trimedoxime, obidoxime, and asoxime)
and diazepam. Since the introduction of the antidotes in treating
the patients poisoned with OPs, there is still no agreement
on how these substances should be given for the best result
following treatment. While the use of atropine and diazepam
in humans have been widely accepted throughout the world.,
Pyridiniumoximes were successful in the treatment of most
cases of OP poisoning, when given with atropine and diazepam.
However, some reports indicate that treatment with pralidoxime
was not sufficiently beneficial. These problems of effectiveness
of oxime treatment may be solved in randomized clinical trial(s)
comparing the WHO-recommended regimen with a placebo to
assess the value of pralidoxime, and other oximes (obidoxime,
trimedoxime, and Asoxime) as well, in acute poisoning with OPs.
Acknowledgement
Vivek Kumar Gupta is grateful to the University Grant
Commission, New Delhi, for providing financial assistance in the
form of a Research Fellowship.
For
more Open Access Journals in Juniper Publishers please
click on: https://juniperpublishers.com
For more articles in Anatomy Physiology & Biochemistry International Journal please click
on: https://juniperpublishers.com/apbij/index.php
For more Open Access Journals please click on: https://juniperpublishers.com
To know more about Juniper Publishers please click on: https://juniperpublishers.business.site/
For more articles in Anatomy Physiology & Biochemistry International Journal please click
on: https://juniperpublishers.com/apbij/index.php
For more Open Access Journals please click on: https://juniperpublishers.com
To know more about Juniper Publishers please click on: https://juniperpublishers.business.site/


Comments
Post a Comment